Medicare’s 8 Minute Rule is a crucial concept in medical billing for therapists, particularly those working with Medicare patients. It governs how time-based therapy services are billed and reimbursed. In this article, we will break down everything you need to know about the 8 Minute Rule from its purpose and history to how to calculate billable units correctly.
What Is the Medicare 8 Minute Rule?
Core Purpose and Origin
The Medicare 8 Minute Rule was designed to standardize the billing process for time-based therapy services, ensuring that healthcare providers can be reimbursed fairly for their work while preventing overbilling. It primarily applies to physical therapy (PT), occupational therapy (OT), and speech-language pathology (SPL). This rule ensures that therapists are compensated for the actual time spent providing services, while also establishing clear guidelines for billing and reimbursement.
Key Governing Bodies (CMS, AMA)
The Centers for Medicare and Medicaid Services (CMS) is the primary governing body that sets rules for Medicare, including the 8 Minute Rule. The American Medical Association (AMA) also plays a role in defining codes and reimbursement practices for healthcare services, including therapy services. These organizations set the framework that defines how the 8-Minute Rule applies to billing, making it essential for providers to stay updated with their regulations.
Services Covered (PT/OT/SPL)
The Medicare 8 Minute Rule applies to three primary therapy services:
- Physical Therapy (PT): Treatment to restore mobility and function.
- Occupational Therapy (OT): Therapy to help patients regain daily life skills.
- Speech Language Pathology (SPL): Treatment for speech and language disorders.
These services are eligible for reimbursement under Medicare Part B when billed according to the 8Minute Rule guidelines.
Why the 8 Minute Rule Exists
Preventing Overbilling & Fraud
By defining minimum time thresholds for billing therapy services, the rule prevents providers from submitting claims for time not actually spent with patients, reducing potential fraud. It also offers a framework that can be applied in other medical billing contexts, such as Hospitalist Billing Services, where precise documentation and time-based billing practices are equally critical for compliance and accurate reimbursement.
Standardizing Time-Based Reimbursement
Before the 8 Minute Rule, billing for therapy services was more subjective. The introduction of the rule helped to standardize the process, ensuring that all providers follow the same procedures when calculating and billing for therapy time. This reduces the chances of errors and discrepancies in billing practices.
Ensuring Medical Necessity
The rule also ensures that services provided under Medicare are medically necessary. By tracking the exact time spent providing services, Medicare can assess whether the amount of therapy being provided is justified based on the patient’s needs. It ensures that resources are allocated properly and only when required.
Who Must Follow This Rule?
Applicable Providers (Therapists, Clinics, Hospitals)
The 8 Minute Rule applies to a wide range of healthcare providers involved in time-based therapy services. These include:
- Therapists: Physical therapists, occupational therapists, and speech-language pathologists.
- Clinics and Hospitals: Institutions that offer therapy services to Medicare patients must comply with the 8 Minute Rule.
Providers who fail to comply with the rule could face reimbursement delays or denials from Medicare.
Payer Types (Medicare Part B, Medicaid, TRICARE)
While the Medicare 8 Minute Rule applies primarily to Medicare Part B, other payers such as Medicaid and TRICARE may have similar billing structures in place. However, it’s essential to check with each payer for specific rules and guidelines related to time-based services.
Exempt Services (Evaluations, Group Therapy)
Certain services are exempt from the 8 Minute Rule. These include:
- Evaluations: Initial assessments and evaluations are not subject to the 8 Minute Rule.
- Group Therapy: Group therapy sessions are typically billed differently, often using a different methodology than individual therapy.
Timed vs. Untimed CPT Codes Demystified
The 8 Minute Rule specifically applies to timed codes, which are used to calculate reimbursement based on the actual time spent providing therapy. Let’s look at the distinction between timed and untimed codes.
List of Common Timed Codes (97110, 97530, 97140)
- 97110: Therapeutic exercises (e.g., strengthening exercises).
- 97530: Therapeutic activities (e.g., balance training).
- 97140: Manual therapy techniques (e.g., joint mobilization).
These are billed based on the time spent on each service, which is where the 8-Minute Rule applies.
Untimed/Service-Based Codes (97001, 97750, 97164)
Untimed or service-based codes, on the other hand, are not dependent on the time spent. These include:
- 97001: Physical therapy evaluation.
- 97750: Physical performance test.
- 97164: Re-evaluation.
For these services, reimbursement is typically a flat rate regardless of time spent on the procedure.
Modifiers for Combined Services (GP, GO)
When multiple services are provided in one session, modifiers such as GP (Physical Therapy) and GO (Speech Therapy) are used to indicate which type of therapy was provided. These modifiers ensure accurate billing for mixed services.
Step-by-Step Unit Calculation
Now that we understand the basics of the 8 Minute Rule, let’s break down how to calculate billable units correctly.
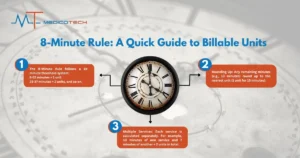
The 15-Minute Threshold System
The 8 Minute Rule operates within a 15-minute threshold system. Each unit of therapy is calculated based on the total number of minutes spent providing therapy. For example, 8-22 minutes counts as 1 unit, 23-37 minutes counts as 2 units, and so on.
Remainder Math Explained (8+ Minutes = 1 Unit)
The rule rounds up any remaining minutes to the nearest unit. For instance, if a therapist provides 13 minutes of therapy, it’s rounded up to 1 unit. Similarly, 22 minutes is considered 1 unit, but 23 minutes rounds up to 2 units.
Multi-Service Session Examples
When multiple services are provided in one session, the 8 Minute Rule requires that each service be calculated separately. For example, if a therapist provides 10 minutes of one service and 7 minutes of another, the total becomes 1 unit for the first service (10 minutes) and 1 unit for the second service (7 minutes), totaling 2 units.
8 Minute Rule Cheat Sheet
Here’s a quick reference table to help with unit calculations:
Total Timed Minutes
Billable Units
8-22
1
23-37
2
38-52
3
53-67
4
Mixed Remainder Calculation (e.g., 5min + 6min = 1 Unit)
If a therapist provides services for 5 minutes and 6 minutes in the same session, the total 11 minutes is considered 1 unit.
Advanced Billing Scenarios
Concurrent vs. Sequential Services
In therapy, services can either be concurrent or sequential, and this distinction is crucial for billing purposes under the 8 Minute Rule.
- Concurrent Services: These involve providing therapy to two or more patients at the same time. Billing for concurrent services under the 8 Minute Rule can be tricky, as you must ensure that the time spent with each patient is accurately tracked and billed. Typically, concurrent therapy is billed using a modifier to indicate that multiple patients were treated at the same time.
- Sequential Services: These involve providing therapy to one patient at a time. Since sequential services are provided to only one patient, the time spent on each unit is more straightforward to calculate and follow the traditional 8 Minute Rule.
Telehealth Sessions (Modifier 95)
The rise of telehealth services has led to new challenges in applying the 8 Minute Rule. For telehealth sessions, you must use Modifier 95, which indicates that the service was provided via telecommunication technology. The time spent on telehealth sessions is calculated just like in-person visits, but using this modifier ensures that the service is correctly billed and reimbursed under Medicare Part B.
Partial Units in Commercial Insurance
Commercial insurance policies may have different guidelines for billing therapy services. Unlike Medicare, some commercial payers don’t follow the 8 Minute Rule exactly and may allow billing for partial units. This could involve billing for fractions of a unit based on the total therapy time, depending on the insurance company’s policies. Understanding these differences is key to maximizing reimbursement.
Compliance Pitfalls & Audit Risks
Top Documentation Errors
One of the most common pitfalls providers encounter is improper documentation. For the 8-Minute Rule to be followed accurately, all therapy sessions must be thoroughly documented, showing:
- The exact time spent on each therapy modality.
- The therapy codes used.
- Whether concurrent or sequential services were provided.
Failure to document appropriately can lead to audit risks, especially when the billed time doesn’t align with what is recorded.
Time Tracking Best Practices
Accurate time tracking is essential for compliance with the 8 Minute Rule. Providers should:
- Use digital timers to track therapy sessions, ensuring precise calculation of time spent.
- Implement a system for manual documentation in case digital tools fail or are unavailable.
- Regularly review time logs to ensure no discrepancies exist before submission.
Medical Necessity Linking
For Medicare to reimburse services, medical necessity must be demonstrated. The therapy provided should align with the patient’s documented needs, and there must be a direct link between the treatment provided and the patient’s diagnosis. Failure to link the services to medical necessity is a common audit red flag.
8 Minute Rule vs. AMA Rule of Eights
Medicare (Aggregate Time) vs. Commercial (Per-Code)
The 8 Minute Rule under Medicare aggregates total time across all therapy sessions, meaning multiple therapy modalities can be combined to meet the required thresholds for billing. In contrast, the AMA’s Rule of Eights typically applies to commercial insurance, which often uses per-code billing, meaning each therapy code is billed separately based on time spent on that specific code.
“Substantial Portion” Methodology
The AMA Rule of Eights allows for billing based on a “substantial portion” of time. If a service is provided for a substantial portion of a unit (e.g., 7 minutes for a 15-minute unit), some commercial insurers may allow billing for that fraction. However, under Medicare’s 8-Minute Rule, you cannot bill for less than 8 minutes of service.
Tools for Error-Free Implementation
EMR Billing Calculators (WebPT, Raintree)
Electronic Medical Record (EMR) systems like WebPT and Raintree come equipped with billing calculators that simplify 8 Minute Rule compliance. These calculators automatically track time, calculate units, and generate bills, reducing the risk of errors. Using such systems ensures accuracy and saves time.
Automated Time-Tracking Software
Time-tracking software, such as Clockify or Trello, can help track therapy time efficiently. These tools can log session durations, automate calculations, and generate reports that ensure compliance with the 8 Minute Rule. These tools are especially helpful in multi-service sessions, where accurate time tracking is crucial.
Free Downloadable Worksheets
For smaller practices or those looking for a more manual approach, many websites offer free downloadable worksheets for calculating billable units. These worksheets typically include tables and formulas for easy reference and ensure providers stay compliant with Medicare guidelines.
Frequently Asked Questions
“Can I bill for 7 minutes of therapy?”
Under the 8 Minute Rule, you cannot bill for 7 minutes of therapy. A minimum of 8 minutes is required to bill for 1 unit. Therefore, you need to round up time to the nearest 8 minute increment.
“Does this apply to Medicare Advantage?”
Medicare Advantage plans often follow similar guidelines to Medicare Part B, but there may be some differences. It’s essential to check with the specific Medicare Advantage provider to ensure compliance with their time-based billing policies.
“How to bill 1-on-1 vs. concurrent care?”
For 1-on-1 care, you bill for the total time spent with each patient individually. For concurrent care, you must split the total session time and apply modifiers to indicate the therapy provided to multiple patients at once. The 8 Minute Rule applies to both types of care, but billing for concurrent care can be more complex.