There is a wide range of CPT codes associated with the therapeutic, prophylactic or diagnostic efforts performed by injections, but one of the most frequently used ones is CPT Code 96372. Such injections are given either subcutaneously (under the skin) or intramuscularly (into the muscle), and it is important to learn the entire range of this code to make a proper billing, documenting, and receiving the corresponding reimbursement. This guide will include all that you need to know about CPT Code 96372 in detail, its definition, when to use it, how to bill it, its frequent denials, and how to ensure that you can work in compliance with reimbursement policies.
What Is CPT Code 96372? Official Definition
AMA’s Official Definition
According to the American Medical Association (AMA), CPT Code 96372 is used for the administration of a therapeutic, prophylactic, or diagnostic injection. These injections are typically delivered subcutaneously (under the skin) or intramuscularly (into the muscle), as opposed to intravenous (IV) injections which are billed under a different code.
Layman’s Explanation:
In simpler terms, CPT Code 96372 refers to any type of injection a doctor gives you to treat, prevent, or diagnose a condition. These injections can be for a variety of reasons, such as relieving pain, managing allergies, or administering hormones. It’s important to note that this code is not used for IV injections or vaccinations, which have their own specific billing codes like CPT 90471 for vaccinations.
When to Use CPT 96372? Approved Clinical Scenarios
Common Uses for CPT 96372
This code is appropriate in a wide range of scenarios where subcutaneous or intramuscular injections are administered. Some common examples include:
- Pain Management: Administering pain-relieving injections like Toradol for acute pain.
- Allergy Treatments: Allergy shots (e.g., desensitization injections) used for conditions such as hay fever or allergic rhinitis.
- Hormonal Injections: Hormonal therapy such as testosterone or birth control injections.
- Antibiotics: Injecting antibiotics like penicillin or other medications for treating infections.
Scenarios Where CPT 96372 Does Not Apply
- IV Infusions: CPT 96372 should not be used for intravenous (IV) infusions. These should be billed using CPT Code 96374 for IV push medications or other specific codes for IV infusion services.
- Vaccines: Injections used for vaccinations are billed under CPT Code 90471, not CPT 96372.
How to Bill CPT 96372 Correctly
Proper billing practices are essential to avoid denials and ensure that your practice receives appropriate reimbursement. Below are detailed guidelines for billing CPT Code 96372.
Step-by-Step Billing Guidelines
Drug + Administration Billing
When billing for CPT 96372, it’s essential to include the drug’s J-code (a specific code assigned to the drug being administered). This code ensures that the exact medication administered is recorded and billed correctly.
- J-codes: Each drug administered via injection has a corresponding J-code that must be included on the claim form. For instance, J-codes are used to represent the specific drug being injected, such as J1885 for Toradol.
Modifiers for CPT 96372
There are instances where you will need to use modifiers to indicate that the injection was provided as a separate service. These are the most commonly used modifiers:
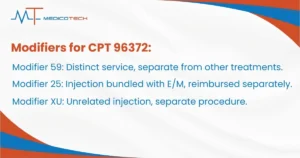
- Modifier 59: Used to indicate that the service is distinct or separate from other services on the same date. This modifier is essential when the injection is given alongside other treatments.
- Modifier 25: When CPT 96372 is bundled with an Evaluation and Management (E/M) visit, use Modifier 25 to indicate that the injection was a distinct service and should be reimbursed separately.
- Modifier XU: This modifier is used when the injection is unrelated to other services provided on the same day, helping to differentiate the two procedures.
Correct Unit Billing
For each CPT 96372 injection, you should only bill one unit unless multiple injections are given. One unit equals one injection.
Avoiding Denials: Top 5 Common Billing Mistakes
Proper billing is critical to avoid claim denials, and there are several common errors that can lead to the rejection of your claim for CPT 96372. Here are the top mistakes to watch out for:
- Bundling Errors: CPT 96372 should not be bundled with certain other procedures, especially E/M services. If you provide an E/M service and an injection on the same day, use Modifier 25 to unbundle the services and get reimbursed for both.
- Incorrect Route of Administration: CPT 96372 is specifically for subcutaneous and intramuscular injections. If you are administering an IV injection, you must use a different code (e.g., CPT Code 96374 for IV push).
- Missing Modifiers: If you are required to use a modifier (e.g., Modifier 59, Modifier 25, or Modifier XU) and fail to include it, your claim could be denied.
- Duplicate Billing: Make sure that you are not submitting multiple claims for the same procedure. Always check that no duplicate claims are filed for a single injection.
- Incorrect Quantity: For CPT 96372, ensure that only one unit is billed per injection. If multiple injections are given, you may bill additional units, but each injection must be clearly documented.
Documentation & Compliance: Key Requirements
Medical Record Requirements
Documentation is key to ensuring compliance with payer policies and avoiding claim denials. Be sure that the following information is clearly documented in the patient’s medical record:
- Drug Name: Specify the medication administered.
- Dose: Include the exact dosage of the drug.
- Route of Administration: Indicate whether the injection was subcutaneous (SubQ) or intramuscular (IM).
- Medical Necessity: Include a note explaining why the injection was necessary, linking it to the patient’s diagnosis.
- Injection Site: Document the specific location of the injection (e.g., left deltoid, right thigh).
Audit-Proofing Your Claims
To reduce the risk of audit issues, always make sure that the ICD-10 codes are properly linked to the CPT 96372 code. The diagnosis codes should correlate with the reason for administering the injection. This helps ensure that your claim is medically necessary and compliant with payer guidelines.
96372 Reimbursement & Payer Policies
Reimbursement rates for CPT 96372 can vary by payer, including Medicare, Medicaid, and private insurers. It is important to stay up-to-date on each payer’s policies to maximize reimbursement.
2025 Fee Schedule: Medicare & Commercial Payer Comparisons
National reimbursement rates for CPT 96372 typically range from $20 to $25 per injection. However, these rates can vary by payer and geographic location. Medicare and commercial insurers may offer different reimbursement rates, so it’s important to check with each payer to determine the exact rates.
Maximizing Reimbursement
To maximize reimbursement for CPT 96372, ensure that all documentation is complete and accurate. If a claim is denied, follow the appeals process to provide additional supporting documentation. Be proactive in appealing denials, and consider consulting payer-specific policies for further guidance.
96372 vs. Other Injection Codes
CPT 96372 vs. CPT 96374 (IV Push)
- CPT 96372 is for subcutaneous or intramuscular injections.
- CPT 96374 is used for intravenous (IV) push medications. These two codes are not interchangeable. Always ensure that the correct route of administration is used when selecting the appropriate code.
CPT 96372 vs. CPT 96401 (Chemotherapy)
- CPT 96372 is used for non-chemotherapy injections, including pain management, antibiotics, and hormones.
- CPT 96401 is used specifically for chemotherapy injections, so it should only be used for chemotherapy drugs.
Frequently Asked Questions (FAQs) About CPT 96372
Can 96372 be billed with vaccines?
No, CPT 96372 cannot be billed for vaccines. Vaccinations are billed under CPT Code 90471 or other appropriate codes depending on the vaccine.
How many units should be billed for a single injection?
Typically, one unit of CPT 96372 should be billed per injection. If multiple injections are given, additional units may be billed.




