What is CPT Code 90837?
CPT Code 90837 is a billing code used for psychotherapy sessions that last 53 minutes or more. It is used by healthcare providers, including psychologists, social workers, and therapists, to bill for intensive psychotherapy sessions aimed at treating complex mental health conditions like depression, trauma, and anxiety. This code ensures that longer, more focused sessions are reimbursed appropriately.
Clinical Scope: Psychotherapy for Complex Cases
CPT Code 90837 is specifically designed for longer psychotherapy sessions for patients with complex conditions. It is ideal for patients suffering from conditions such as:
- Post-Traumatic Stress Disorder (PTSD)
- Severe Major Depression
- Bipolar Disorder
- Anxiety and Trauma-related Disorders
These sessions require more time and therapeutic focus, addressing significant emotional challenges that shorter sessions cannot adequately manage.
Key Distinction: 90837 vs. 90834 vs. 90832
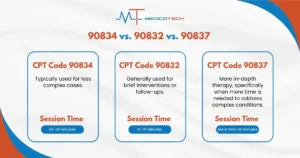
CPT Code 90837 is often compared to other therapy codes based on session length and complexity:
- CPT Code 90834 is for 45-50 minute sessions, typically used for less complex cases.
- CPT Code 90832 applies to 16-37 minute sessions, generally used for brief interventions or follow-ups.
- CPT Code 90837 is used for longer, more in-depth therapy, specifically when more time is needed to address complex conditions.
Time Requirements & Session Structure
Minimum Time Threshold: 53+ Minutes
For CPT Code 90837, the session must last at least 53 minutes. This minimum requirement ensures that the session provides enough time to address complex therapeutic needs and that it complies with billing standards.
Medicare’s 53-Minute Rule Explained
Under Medicare guidelines, a psychotherapy session billed with CPT Code 90837 must last a minimum of 53 minutes. This excludes any time spent on administrative duties or documentation. The focus must be on direct therapeutic interaction with the patient during this time.
Documenting Start/End Times Correctly
Accurate documentation of session times is critical. Healthcare providers should clearly document both the start and end times of the session to demonstrate that the 53-minute requirement is met. This helps avoid billing issues and ensures compliance with Medicare and other insurance policies.
Medical Necessity & Clinical Justification
When to Bill 90837: Approved Use Cases
CPT Code 90837 should be used when a longer therapy session is required for patients with complex mental health conditions. Typical use cases include:
- Severe Depression and PTSD where extended therapy is necessary
- Chronic mental health conditions that cannot be adequately addressed in shorter sessions
- Crisis intervention where intensive therapeutic engagement is needed
Qualifying Diagnoses (e.g., F43.10 PTSD, F33.2 Major Depression)
This code is primarily used for patients diagnosed with severe conditions such as:
- F43.10: PTSD
- F33.2: Major Depressive Disorder, Recurrent, Severe
- F31.3: Bipolar Disorder, Most Recent Episode Depressed
These conditions often require extended sessions to make meaningful therapeutic progress.
Avoiding Upcoding: Red Flag Scenarios
Upcoding can occur when a provider bills for a service that was not provided. For example, billing for CPT Code 90837 when a session lasted less than 53 minutes can trigger audits and potential denials. Providers should ensure that the session length and clinical justification align with the billing code.
Documentation Essentials
Required Note Components (SOAP Format)
Proper documentation is essential to justify the use of CPT Code 90837. The SOAP format is commonly used for this purpose:
- S (Subjective): Patient’s reported feelings and symptoms.
- O (Objective): Therapist’s observations and assessments.
- A (Assessment): Evaluation of the patient’s progress or challenges.
- P (Plan): Detailed therapeutic interventions used and planned next steps.
This format ensures comprehensive session notes, which are critical for medical necessity and insurance claims.
Proving Medical Necessity in Records
When billing for CPT Code 90837, therapists must provide clear evidence of medical necessity. This includes showing why the patient requires an extended session and how the patient’s diagnosis supports the need for longer therapy. Documentation should outline the patient’s symptoms and treatment progress, indicating that shorter sessions would not suffice.
Audit-Proof Documentation Strategies
To avoid audits, providers should:
- Accurately document session start and end times
- Include clear treatment goals and objectives for each session
- Ensure the session duration meets the 53-minute minimum
- Justify the medical necessity of the extended session in the patient’s records
Reimbursement & Financial Insights
2025 Medicare Fee Schedule ($154.29 national avg)
In 2025, the national average reimbursement for CPT Code 90837 under Medicare is approximately $154.29. This amount can vary depending on geographic location and specific contractual agreements with insurance companies. Providers should always check the current fee schedule to ensure that their claims are accurately reimbursed.
Commercial Payer Variations (Blue Cross, UHC, etc.)
For commercial insurance plans, such as Blue Cross or UnitedHealthcare, reimbursement for CPT Code 90837 can vary significantly. It’s crucial to understand the payers’ policies and ensure compliance with their specific requirements. Out-of-network providers may receive lower reimbursements, so understanding these details is essential for maximizing revenue.
Maximizing Reimbursement Legally
Providers should maximize reimbursement for CPT Code 90837 by:
- Ensuring accurate documentation of session length and medical necessity
- Adhering to insurance and Medicare billing rules
- Reviewing payer-specific reimbursement rates and adjusting billing practices accordingly
- Avoiding upcoding or downcoding, which can negatively affect reimbursement rates and cause legal issues.
VI. Billing Compliance & Modifiers
Telehealth Billing: Modifier 95 + POS 02
With the increasing demand for telehealth services, CPT Code 90837 can be billed for telehealth sessions, but specific modifiers must be used to ensure proper reimbursement. For telehealth sessions, the Modifier 95 should be appended to the code to indicate that the session occurred via telecommunication technology. Additionally, Place of Service (POS) code 02 should be used to reflect that the service was provided in a telehealth setting.
This combination of Modifier 95 and POS 02 ensures that the insurance company recognizes the session as a legitimate telehealth service and reimburses it accordingly. Providers should check with individual insurers for their telehealth reimbursement policies, as not all payers may cover telehealth sessions at the same rates or under the same conditions.
Interactive Complexity Add-On (90785)
In some psychotherapy sessions, interactive complexity may be present, which makes the session more complex and time-consuming. The Interactive Complexity Add-On (CPT Code 90785) should be billed alongside CPT Code 90837 if the session involves additional challenges, such as:
- Communication barriers (e.g., language or hearing difficulties)
- Patient’s family involvement that requires additional therapy coordination
- Co-occurring issues like severe substance abuse or severe personality disorders
Adding 90785 to CPT Code 90837 can increase reimbursement, as it acknowledges the additional complexity and time required to conduct the therapy session. It’s essential to accurately document the circumstances that justify the use of this modifier.
Crisis Code Combinations (90839/90840)
For patients experiencing acute crises, CPT Codes 90839 and 90840 are used in combination with CPT Code 90837. These codes are used to address crisis intervention therapy:
- CPT Code 90839 is for psychotherapy sessions lasting 60 minutes or more to address a crisis situation.
- CPT Code 90840 is for each additional 30 minutes of psychotherapy.
If the therapy session is focused on managing a mental health crisis, these codes should be used in conjunction with CPT Code 90837 to capture the complexity and duration of the intervention.
VII. Payer-Specific Policies
UnitedHealthcare’s 90837 Scrutiny
UnitedHealthcare (UHC) is one of the major insurance providers that may scrutinize the use of CPT Code 90837 to ensure it is being billed correctly. UHC may audit claims to verify:
- That the session duration exceeds the minimum required 53 minutes
- That medical necessity is clearly documented for complex cases
- That the session is appropriately classified as individual psychotherapy rather than a less intensive service
To ensure reimbursement, providers should be meticulous about session documentation and ensure that they follow all specific UHC billing guidelines.
Medicare LCD L33252 Requirements
Medicare Local Coverage Determination (LCD) L33252 outlines the criteria for billing psychotherapy services in specific regions. When billing for CPT Code 90837, providers must comply with Medicare’s medical necessity requirements, which include:
- Clearly documenting that the long duration of the session is required due to the patient’s mental health diagnosis.
- Justifying that shorter sessions would not meet the patient’s therapeutic needs.
- Adhering to the specific documentation standards outlined in the LCD, including detailed progress notes and treatment goals.
Providers should review the LCD guidelines specific to their region to ensure compliance and avoid potential claim denials.
Prior Authorization Trends
Some insurers require prior authorization for CPT Code 90837 to ensure that the extended psychotherapy session is medically necessary. This trend is particularly common with large commercial insurers and Medicare Advantage plans. Providers should be aware of the prior authorization policies for their specific payer to avoid delays in reimbursement. Failure to obtain prior authorization can result in denied claims or delayed payments.
VIII. Audit Risks & Mitigation
Common Billing Errors Triggering Audits
Billing errors are a significant risk when using CPT Code 90837. Common errors that may trigger audits include:
- Underbilling: Submitting claims for shorter sessions (e.g., 50 minutes) when billing for CPT Code 90837, which requires 53 minutes or more.
- Upcoding: Billing for CPT Code 90837 when the session did not meet the required medical necessity or time threshold.
- Incomplete Documentation: Failing to provide adequate session notes, including start and end times, the clinical justification for the extended session, and details of the therapeutic interventions used.To mitigate audit risks, providers should ensure that all documentation is accurate, that the time requirements are strictly followed, and that medical necessity is clearly outlined in the patient’s records.
Navigating Denials & Appeals
If a claim for CPT Code 90837 is denied, providers should carefully follow the appeals process. Common reasons for denial may include:
- Incorrect coding or missing modifiers (e.g., Modifier 95 for telehealth)
- Insufficient medical necessity documentation
- Session duration not meeting the required 53 minutes
To successfully appeal, providers should:
- Review the denial reason and identify the root cause
- Submit additional documentation, such as progress notes, to support the necessity of the extended session
- Follow the payer’s appeal process closely and provide any additional information requested
Frequency Guidelines (How Often to Bill)
Billing CPT Code 90837 for frequent sessions can raise red flags with payers. It’s important to adhere to frequency guidelines based on the patient’s needs and payer policies. For example, Medicare may limit the frequency of certain psychotherapy services, while private payers may have different criteria for how often extended sessions can be billed.
To avoid frequency-related issues, providers should:
- Ensure that extended sessions are medically necessary on a case-by-case basis
- Keep track of the frequency of billing to ensure it aligns with the patient’s treatment plan and payer guidelines
IX. Frequently Asked Questions
“Can I bill 90837 for 50 minutes?”
No, CPT Code 90837 requires the therapy session to last a minimum of 53 minutes. Billing for a session lasting only 50 minutes would be considered underbilling and could result in a denial or audit. Ensure that the session duration meets the minimum threshold to avoid issues with reimbursement.
“Is 90837 covered for group therapy?”
No, CPT Code 90837 is specifically for individual psychotherapy sessions. It is not applicable for group therapy. Group therapy requires a different set of codes (e.g., 90853 for group psychotherapy) and cannot be billed under CPT Code 90837, which is reserved for individual sessions lasting 53 minutes or more.
“How to handle partial sessions?”
If a session falls short of the required 53 minutes but is still medically necessary, it should not be billed under CPT Code 90837. Instead, you should choose an appropriate billing code based on the actual session length (e.g., CPT Code 90834 for 45-minute sessions). It’s essential to accurately document the reason for the shortened session to avoid issues with compliance and reimbursement.




