If you work in medical billing or healthcare administration, you’ve likely encountered a CO 50 denial at some point. These denials can be frustrating and confusing for healthcare providers and billing professionals alike. However, understanding the cause of a CO 50 denial and knowing how to fix it can significantly streamline the claims process. In this article, we will delve deep into CO 50 denials, offering insights into what they are, why they occur, how to resolve them, and steps to prevent them in the future.
What is CO 50 Denial?
CO 50 denial is a commonly seen rejection code in the healthcare industry. It generally refers to an issue with the claim where the insurance company has determined that the services provided were not deemed medically necessary for the patient. This is one of the more frequent denials encountered in the medical billing process, particularly when it comes to health insurance claims.
CO 50 denials specifically indicate that the insurer has reviewed the submitted claim and found that the services rendered fall outside of their coverage guidelines or are not required based on the patient’s condition. This denial often appears in private insurance claims, but can also occur in government programs like Medicare or Medicaid under certain circumstances.
Why Does CO 50 Denial Occur?
Understanding why CO 50 denials occur can help healthcare providers avoid them in the future. Typically, this type of denial occurs when the payer believes that the treatment or service provided was not necessary based on the medical criteria, patient’s history, or guidelines of the insurance policy. The denial can happen for a variety of reasons, all of which are crucial to address in the claim resubmission process.
Reason s for CO 50 Denial
1 Incorrect or Missing Information
One of the most common reasons for CO 50 denial is incomplete or incorrect information on the submitted claim. This can include missing patient details, errors in the provider’s identification, or incorrect procedure codes. When any of this information is missing or inaccurate, it may lead to the claim being flagged and denied for failure to meet the payer’s criteria.
2 Lack of Medical Necessity
CO 50 denial often arises due to the insurance company’s determination that the services provided were not medically necessary. Insurers have specific guidelines they follow to determine the medical necessity of a treatment. If the treatment or service is considered to be unnecessary, the insurer will deny the claim, using the CO 50 code to indicate this reason.
3 Timely Filing Issues
If the claim is submitted beyond the insurer’s deadline for filing, it may be denied. Health insurance companies have strict filing deadlines for claims, and claims submitted after these deadlines will typically be denied. Timely filing issues could happen due to delays in obtaining patient information, processing the claim, or even human error.
4 Duplicate Claims
Duplicate claims refer to situations where the same claim has been submitted multiple times, either by mistake or intentionally, in order to obtain payment more than once. If an insurer detects a duplicate claim, it will deny one of them with the CO 50 denial code, as this is a clear violation of billing protocols.
5 Non-Covered Services
Certain services may not be covered under the patient’s specific insurance plan. This is especially common with elective procedures, experimental treatments, or out of network services. If the provider submits a claim for a service that is outside the scope of what is covered by the patient’s plan, the insurer will reject the claim, and it will be flagged as CO 50 denial.
Steps to Resolve CO 50 Denial
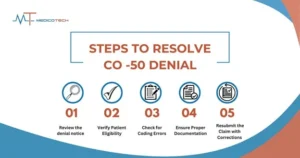
When a CO 50 denial is received, healthcare providers need to take swift action to resolve the issue. Here are some essential steps to follow to fix CO 50 denials.
1 Review the Denial Notice
The first step in resolving a CO 50 denial is thoroughly reviewing the denial notice provided by the insurer. This notice typically includes a detailed explanation of why the claim was rejected. Pay close attention to the specifics outlined in the notice, such as whether the denial was due to lack of medical necessity, incorrect information, or another reason.
2 Verify Patient Eligibility
Ensure that the patient was eligible for the services rendered at the time the treatment took place. This includes confirming the patient’s coverage, policy details, and whether the procedure or service is included in their benefit plan. Sometimes, eligibility issues can be resolved simply by verifying that the patient was covered on the date of service
3 Check for Coding Errors
Billing codes (CPT, ICD, and HCPCS) are crucial for accurate claims submission. Mistakes in coding can result in a CO 50 denial. Review the coding used on the claim to make sure that the services and diagnoses align with what is covered under the patient’s insurance. Additionally, ensure that modifiers are properly used, as they are essential in determining how a claim is processed. With our medical coding services, we ensure that the correct codes are used for diagnoses and procedures, improving claim accuracy.
4 Ensure Proper Documentation
Thorough and accurate documentation is key to supporting a claim. If the insurer is denying the claim for lack of medical necessity, the proper medical documentation should be submitted to support the treatment or services provided. This may include medical records, physician notes, lab results, and other documents that show the necessity of the services rendered.
5 Resubmit the Claim with Corrections
Once you’ve identified and corrected the issue whether it’s an eligibility issue, coding error, or documentation gap resubmit the claim with the appropriate corrections. Make sure to include all supporting documentation and any additional information requested by the insurance company to ensure the claim is reconsidered.
Preventing CO 50 Denial
While CO 50 denials can happen to anyone, there are steps healthcare providers can take to reduce the likelihood of these denials. By staying proactive and meticulous, providers can avoid unnecessary claim rejections and streamline the billing process.
1 Regular Staff Training
Ensure that your medical billing and coding staff are consistently trained on the latest insurance policies, coding standards, and claims filing procedures. Regular training can help staff stay updated on any changes in payer requirements and guidelines, reducing the chances of errors that could lead to CO 50 denials.
2 Accurate and Complete Documentation
Accurate and comprehensive documentation is essential to substantiating the need for medical services. All patient interactions, treatment plans, and clinical notes should be detailed and include the rationale for the treatments provided. This documentation will help prove medical necessity if the insurance company questions the claim.
3 Use of Advanced Coding Tools
Investing in advanced coding tools can help minimize the risk of errors. These tools ensure that the correct codes are used for diagnoses and procedures, improving claim accuracy. Moreover, some tools come with built-in checks to verify whether a procedure is covered by insurance and can assist in identifying any coding mistakes before submission.
4 Conducting Regular Audits
Implement regular audits of your medical billing process to ensure that all claims are submitted accurately and within guidelines. Audits can help identify trends in denials, such as recurring CO 50 denials, and highlight any patterns in coding or documentation errors.
5 Seeking Professional Help
If your practice is frequently experiencing CO 50 denials, it might be time to consult with a medical billing expert. These professionals have extensive experience in navigating the complexities of medical billing and can help you resolve issues more efficiently.
When to Consult a Medical Billing Expert
Consulting a professional can provide many benefits, especially if CO 50 denials become a recurring issue. Medical billing experts are skilled at identifying errors that may be hard to spot and have established relationships with insurance companies. They can help with:
- Correcting coding and documentation errors
- Navigating payer guidelines and protocols
- Dealing with repeated denials efficiently
- Handling complex billing issues
Benefits of Outsourcing Medical Billing
Outsourcing medical billing to a dedicated service provider offers several advantages:
- Expertise: Professional billing services have deep knowledge of payer-specific guidelines and industry standards, ensuring claims are filed correctly the first time.
- Time Saving: Outsourcing allows healthcare providers to focus on patient care, while the billing service handles all the claim submissions and follow-ups.
- Improved Cash Flow: A billing expert can help reduce denials, ensuring claims are paid faster and more consistently, leading to improved revenue flow.
Conclusion
Recap of Key Points
In summary, CO 50 denials are a common occurrence in medical billing, typically related to the lack of medical necessity of services rendered. To resolve CO 50 denials, it is important to review the denial notice, verify patient eligibility, check for coding errors, ensure proper documentation, and resubmit the corrected claim. Additionally, taking steps to prevent CO 50 denials such as regular staff training, maintaining accurate documentation, and using advanced coding tools can help reduce the risk of these denials in the future.
Final Thoughts on Managing CO 50 Denial
Managing CO 50 denials can be challenging, but with the right approach, it is possible to fix these denials and prevent them from recurring. By being proactive, investing in training and tools, and seeking professional help when necessary, healthcare providers can ensure their billing process runs smoothly and their claims are processed correctly. Whether you handle billing in house or outsource to an expert, the key to managing CO 50 denials is staying informed, organized, and thorough in every step of the process.




