Rheumatology
Billing Services
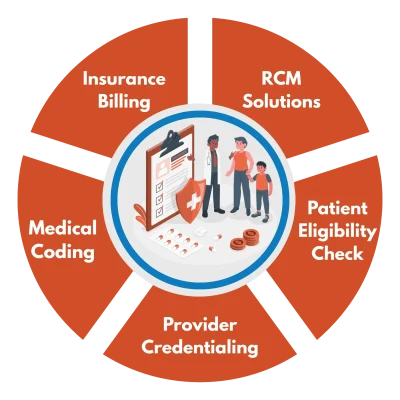
Medicotechllc is a HIPAA-compliant Rheumatology billing company offering end-to-end RCM solutions. We handle everything from complex coding for Synovectomy and Joint Replacement Surgery to Plasmapheresis. Trust us as your Rheumatology billing services provider and experience growth and timely reimbursements.
Benefits of Outsourcing Rheumatology Billing Services
There are several reasons for choosing an outsourced billing company, but the most prominent are affordability and efficiency. Outsourcing allows you to reduce costs associated with hiring, managing, and paying salaries. Additionally, it gives you access to certified, experienced professionals who focus on faster claim processing and improved financial performance, along with all the necessary resources. Furthermore, outsourcing ensures compliance and supports the scalability of your practice.
Outsource your rheumatology billing to Medicotechllc and focus on delivering excellent patient care.

Medical Coding
According to the AMA, the average medical practice submits more than 50% of its claims with incorrect codes. Inexact and inconsistent coding increases the risks of undercharging, overcharging and post-payment audit.
At PGM, all of our clients undergo a practice evaluation where our certified coders, in conjunction with our reimbursement specialists, analyze practice procedures and codes to make recommendations that ensure accurate and optimum reimbursement.
Patient Charge and Demographics Data Entry/Upload
Patient demographics and charges are collected from your office daily. Data can be scanned, faxed or couriered to any one of our locations. Once the data has been received, a dedicated PGM account representative will enter the information into our practice management system.
For PGM clients using an electronic medical record system (EMR/EHR), patient demographics and charge data can be electronically transferred in real-time to our practice management system though our EMR/EHR medical billing interface.
Claims Review
PGM's reimbursement specialists compile and review all client patient and charge data. Billing uploads and batches are balanced, and our medical claims process software is used to 'scrub' claims for errors and omissions. PGM's software performs thousands of checks, including CPT/ICD-9 validations, modifier checks, demographic comparisons and payer-specific edits.
The claims review process ensures that practice billing data is being accurately captured and that claims are clean prior to being submitted for payment. Clean claims greatly increase the rate of payment, helping to maximize the amount collected and reduce accounts receivable.
Claim Submission
Once the claims are reviewed and audited, they are transmitted to the various payers for reimbursement. PGM has the ability to electronically transmit claims to thousands of payers nationwide. For those payers that do not have the ability to receive electronic claims, PGM will generate and mail paper claims.
After submission, claims receive an additional level of "scrubbing' by our clearinghouse. Edits and errors are relayed back to PGM for correction.
Payment Posting
Payments are received either hard copy or via electronic remittance advices (ERA). PGM clients are given the option to continue to receive payment at the practice or to have PGM manage all payments at one of our facilities.
Once payment is received, it is reviewed and line-item posted into our practice management system by one of our reimbursement specialists.
Claim Tracking
Once payments have been posted into our practice management system, they are run through our payer-specific rules software, which aggressively detects unpaid or misadjudicated claims.
Once an unpaid or misadjudicated claim is flagged, it is brought to the attention of one of our reimbursement specialists for further investigation and active follow-up.
Denial Management and Follow-up
Only 70% of the average medical practices insurance claims are ever paid by insurance providers. While a practice may submit a perfectly clean claim to a payer, there is no guarantee that it will get paid or, for that matter, get paid accurately.
It's no secret that payers continue to impose increasingly complex rules, systems and loopholes with the single goal of limiting payment. This frequently means that practices remain unpaid on the valuable service provided to patients.
PGM's incentive-based fee structure ensures that we work hard to make sure nothing gets left behind. Once an outstanding claim has been identified as past due, PGM's system alerts our account representative who then reviews the history and follows up on the claim accordingly.
Patient Balances Billing
At PGM, we understand that patients are the lifeblood of the practice. We work directly with the practice to custom tailor a patient billing profile to perform all patient billing functions on behalf of the practice.
The typical patient billing profile includes a series of easy to understand statements. Should a patient fail to make payment, additional letters and/or a call sequence is initiated. For questions regarding a bill, patients are provided a toll-free number to call where one of our patient billing specialists is ready to answer any questions.
PGM does not perform collection services, and therefore patient billing services are structured to encourage patients to resolve outstanding balances. For those patients who refuse or are unable to complete their obligation, PGM will work with the practice to structure a patient payment plan or transition the balance to a third-party collection agency for resolution.
Reporting
PGM provides advanced financial and practice analysis tools designed to give enhanced visibility into practice operations at the click of a button. Practices are provided access to PGM-online, our Internet-based reporting system, where they can access hundreds of practice analysis and performance reports. Should a practice require additional information, custom reports are also available upon request.
Additionally, PGM's reimbursement specialists provide frequent practice performance reviews offering additional insight into practice financial operations.
Specialty Specific Billing
Medicotechllc is dedicated toward making healthcare easy for providers and delivering specialty-specific billing solutions, reducing the errors, denials, delays, and inefficiencies.
✅ Methotrexate
✅ TNF Inhibitors
✅ Hyaluronic Acid Injections
✅ JAK Inhibitors
✅ IVIG Therapy
✅ Synovectomy
✅ Plasmapheresis
✅ Stem Cell Transplantation
HIPAA Compliant Solutions
Medicotechllc follows all payer guidelines and coding standards, including ICD-10 and CPT, with the support of certified coding and billing professionals. We understand the importance of compliance with HIPAA guidelines for every medical facility and billing provider. We ensure compliance with HIPAA guidelines and safeguard PHI to maintain data security.
Patient & Provider Satisfaction
Many billing companies focus solely on providers, neglecting the fact that patients are the core focus and deserve the most attention. We prioritize both patient care and provider satisfaction, ensuring patients receive the care they deserve and providers get every penny for the work they’ve done.
Time Efficient Billing
Poor medical billing isn’t just about claim denials; it’s also about billing on time for better reimbursement rates and practice growth. Time is a valuable resource that cannot be wasted. Our billers understand this, and we create bills that are approved on the first submission. We maintain a 99% first-submission claim approval rate.
Treatments like joint injections and biologic agents may have specific billing guidelines. To avoid denials, they must be billed within the required time-frame.

Out-of-Network Providers Billing Solutions
Biologic medications are costly when provided by out-of-network rheumatologists or infusion centers; these treatments can result in significant financial burden for patients and complications in billing services. Providers face challenges with prior authorizations, complex joint injection billing, and uncertainty in coverage for new treatments. Medicotechllc has trained professionals knowing how to navigate these complexities, secure accurate reimbursements, manage long-term treatment plans, and minimize patient out-of-pocket costs, ensuring smooth and efficient claim management.
Billing Nationwide For Multiple Specialties
Managing billing across multiple specialties can be overwhelming for large healthcare facilities. Let us handle it for you with expert, specialty-specific solutions tailored to your needs. As a trusted Rheumatology Billing Company, we ensure accurate and timely billing. Focus on your practice and leave the billing to us!
Handling EHR, EMR & EDI For Practice
Handling EHR, EMR, and EDI is key to smooth rheumatology billing services. With EHRs and EMRs, patient details are kept accurate and easy to access, so you don’t lose time looking for info. EDI helps us submit claims quickly and get paid faster. Our team knows the ins and outs of billing for things like arthritis and autoimmune treatments, making sure everything’s submitted correctly so you can concentrate on your patients.


Frequently Asked Questions
What are the common billing issues in rheumatology?
Common billing issues in rheumatology include complex coding for biologic medications, out-of-network treatment billing, and frequent claim denials for pre-authorization or incorrect coding.
How do Medicotechllc handle billing for biologic medications in rheumatology?
Medicotechllc handles billing for biologic medications in rheumatology by navigating complex guidelines, securing accurate reimbursements, and minimizing patient out-of-pocket costs through efficient claim management and prior authorization processes.
What are the most common codes used in rheumatology billing?
Common rheumatology billing codes include:
- ICD-10: M05.79 (rheumatoid arthritis), M32.9 (systemic lupus)
- CPT: 20610 (joint injection), 96413 (biologic response modifier administration)
J-Codes: J3430 (methotrexate injection), J1725 (IVIG injection)
How do you deal with out-of-network billing in rheumatology?
Medicotechllc addresses out-of-network billing by working directly with payers to obtain approvals, handling detailed coding for specialized treatments, and ensuring that both providers and patients are not burdened by unexpected costs or delayed reimbursements.
What are the HIPAA compliance requirements for rheumatology billing?
HIPAA compliance for rheumatology billing includes safeguarding patient information, ensuring proper coding and documentation, and securely transmitting data. It also involves adhering to payer guidelines, protecting PHI, and conducting regular audits to maintain confidentiality and security. Hire Medicotechllc for compliant rheumatology billing solutions.
Get in Touch With Us
See our contact page for more information
Head Office
7901 4TH ST N STE 300
St. Petersburg, FL 33702
Email Us
info@medicotechllc.com
Call Us
+1 727 353 2939

