Medical Billing
Services
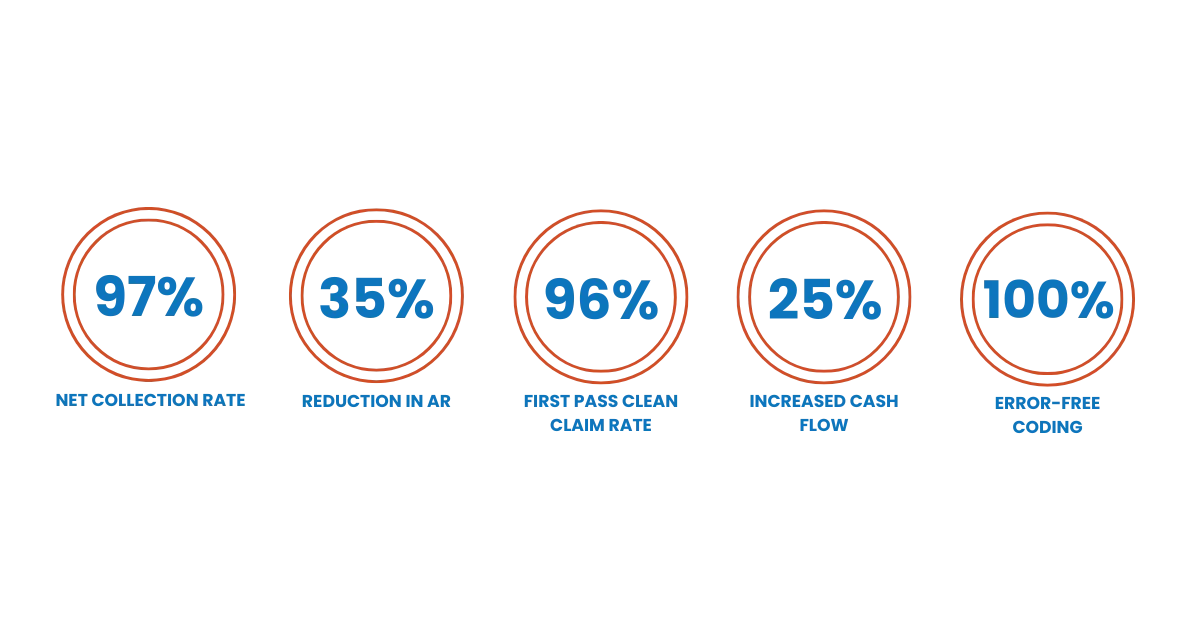
Healthcare providers across the USA lose an estimated $125 billion annually due to billing mistakes, claim denials, and incorrect coding. But with our medical billing service, we guarantee accuracy, minimal claim denials, and error elimination. Over time, this boosts your revenue and lets you focus more on your patients.
Nationwide Expertise In 50+ Specialties, Your Success Starts Here!
End-to-End Medical Billing Service
Having difficulty managing both the patient services and administrative tasks? Why don’t you just focus on one and let us handle the other one? We cover it all, from provider credentialing and patient pre/retro authorization to the final reimbursement deposited into your account. We do it with professionalism, accuracy, and a high success rate. And you can test these claims with the free first-month billing audit we are offering.
Your practice is our expertise; we handle it all for hospitals, clinics, and medical practices.
Why Outsource Medical Billing Services?
In-house medical billing is costly and often leads to mistakes, resulting in claim denials, payment delays, and a negative reputation for your practice. Here’s why outsourcing medical billing services gives you a competitive edge:
- Cost Saving: Outsourcing medical billing can save you money on in-house billing staff, their training, and software expenses, lowering your overall operational costs.
- Faster Insurance Verifications: Made pre/retro authorization easy and fast to ensure you don’t lose patients or face claim delays.
- Error Free Coding & Accuracy: Outsourcing medical billing provides access to skilled professionals who accurately code bills and offer precise, error-free services.
- Industry Regulations & Legal Guidelines: Follow HIPAA compliance and CMS guidelines while staying up to date with ICD-10 coding standards.
- Minimal Claim Rejections: Medical billing expert follows best practices to minimize errors, improving first-pass claim approval rates.
- Advanced Technology & Tools: Access to the latest updated billing software and tools, so you don’t need to invest in them separately.
- Detailed Reports: You receive in-depth analytics and reports on your business’s performance to help you make strategic decisions.
- Maximize Revenue: Fewer claim denials with less operational costs and faster claim submissions means quicker payments and better cash flow.

The Right Medical Billing Partner? You Decide
Business Growth
With Medicotechllc, you can sit back and enjoy your business growth as we accelerate payments by reducing errors, minimizing denials, and compliance with HIPAA, the HITECH Act, CMS guidelines, and ICD-10/CPT/HCPCS coding standards.
Expertise & Experience
We have been providing medical billing and coding services to practitioners for the past five years. Our expert staff is our pride, and by utilizing their skills effectively and training them with the latest standards, we have achieved a 96% success rate in the market.
Stay Aligned & Updated
Our medical billing solutions help you, your staff, and your patients stay aligned. Using the latest technology and software, our system syncs seamlessly with yours to maintain accurate and up-to-date patient data.
Clean Transparent Documentation
Trust is built on consistency and honesty. We keep documentation clear and transparent, ensuring that our clients know exactly how we handle their data and accounts. Getting E&M coding right is a big part of that.
Claim Progress Tracking
We provide real-time tracking and reporting on insurance claims, keeping all parties informed. This streamlines approvals and, through our denial management services, accelerates payments. Stay updated on every step we take to secure your revenue.
Nonstop Customer Care
With our medical billing and consulting services, you receive 24/7 customer support. For us, it’s not just about solving issues; it’s about building trust, reliability, and lasting relationships that keep businesses and customers connected and growing.
Timely Payment Processing
In the end, one of the most important things for a business is receiving the revenue they worked hard for. Keeping its revenue cycle on track and receiving it on time is just as important. That is why we adhere to ERA, EDI, and EFT for secure payments.
Billing Cost
If you outsource medical billing services to Medicotechllc, you can reduce your overall business operational costs by up to 30%, which will eventually scale your profitability.
Factors Affecting the Medical Billing & Revenue

Credentialing and Contracting Delays
Most providers and practices experience contracting delays that impact their revenue due to credentialing, which is the initial and most crucial step for a practitioner to treat insurance company patients. If not done properly, it can result in missed patient opportunities, leading to revenue loss.
Coding Errors and Inaccuracies
Outsource medical billing services no matter the size of your practice, whether you work for one or own it, using manual billing or outdated software without properly trained and professional staff will lead to billing errors, claim rejections, and payment delays.
Regulatory Compliance & Outdated Technology
To avoid any potential legal penalties, a facility must adhere to CMS guidelines, HIPAA regulations, and insurance payer rules. Medicotechllc ensures that practices stay updated and frequently adjust their policies and billing procedures to comply with regulations.

Resolving Claim Denials
We provide services in a way that ensures no claim rejections. However, if a claim is rejected, we have our team of medical billing specialists equipped to handle the issue, resolve the issue, and resubmit the claim for reimbursement.

Payment Delays or Underpayments
Medical services billing payments are often delayed or underpaid due to incorrect coding, lack of accuracy, and untrained staff, resulting in decreased overall revenue. In contrast, professional billing service can improve performance by minimizing errors, maintaining professionalism, and ensuring consistency.
Poor A/R Management
What is poor A/R management? Is it only not receiving claims? No, it’s not only that. Poor A/R management means failing to receive timely reimbursements from insurers, not following up on unpaid claims, incomplete documentation, and not knowing the reasons why, resulting in revenue loss.
Patient Payment Collection Issues
Resolving client issues and streamlining billing processes is our sole mission. We help prevent ineffective patient billing with our unique and proven collection strategies, turning your practice into a reliable cash flow machine.

Prompt Front Desk & Help Desk Services
Efficient front desk and help desk services are the foundation of a practice’s operational success. They are the first impression, shaping the patient’s entire experience. We ensure that accurate and timely information is captured from the very first interaction. This assists providers with patient appointments, data entry, and answering incoming patient calls, allowing clinical staff to focus on patient care. Let us take part and show you how it’s done with expertise, because when this is done right, it significantly reduces the chances of denials and delays.
Smart Digital Medical Billing Solutions
With us, you can grow and streamline your business beyond imagination. How? We effectively manage your administrative tasks with accurate coding and claim submission, and we also handle Electronic Health Records (EHR) to keep you updated and aligned with your patients using the latest technology tools and software. We also handle secondary insurance billing to ensure all claims are processed efficiently. In addition, we create clear and transparent statements that include copays, deductibles, and other patient responsibilities, which increases patient satisfaction and helps them understand their responsibilities to providers.

Frequently Asked Questions
What is EHR in Medical Billing?
EHR (Electronic Health Record) in medical billing is a digital system that stores patients’ medical histories, diagnoses, treatments, and billing information. It helps healthcare providers manage records, streamline coding, and ensure accurate claims submission for faster reimbursements.
What is authorization in medical billing?
Authorization in medical billing is the process of obtaining approval from a patient’s insurance company before delivering specific medical services to confirm coverage. It ensures the provider will be reimbursed and prevents claim denials or patient payment disputes.
What are the 10 steps in the medical billing process?
The 10 steps in the medical billing process are:
- Patient Registration – Collecting patient and insurance details.
- Insurance Verification – Checking coverage and eligibility.
- Charge Entry – Recording services and applying medical codes.
- Claim Generation – Preparing claims for submission.
- Claim Submission – Sending claims to insurance companies.
- Adjudication – Insurers review and process claims.
- Payment Posting – Logging received payments.
- Denial Management – Handling and resubmitting denied claims.
- Patient Billing – Sending invoices for remaining balances, not covered by the insurer.
- Follow-up & Collections – Ensuring outstanding payments are received.
What is pc ratio in medical billing?
The PC ratio (Patient-Claim ratio) in medical billing refers to the number of claims submitted for each patient. For a provider, monitoring the PC ratio is important because it helps ensure that claims are processed correctly, all services provided are billed accurately, and there is no need for additional claim submissions.
Difference between reversal and recoupment in medical billing?
In medical billing, reversal means canceling or voiding a submitted claim or payment before it is finalized, usually due to errors. Recoupment is when an insurance company takes back money already paid to the provider, often by offsetting it against future claims.
Get in Touch With Us
See our contact page for more information
Head Office
7901 4TH ST N STE 300
St. Petersburg, FL 33702
Email Us
info@medicotechllc.com
Call Us
+1 813 393 9744